
Everyone deals with stress. It’s an unavoidable part of life, right? We all feel overwhelmed, maybe a little irritable and completely drained when a huge project lands at work or there’s a tough situation with family.
But here’s the thing: What happens when that feeling simply refuses to leave?
I mean, the project is finally done and the immediate problem is solved, yet you’re still feeling that heavy cloud. I used to think I was just “bad at relaxing.” But that persistent, nagging feeling that something is truly off? That’s an essential signal, and it’s important to pay attention to it.
Of course, a specialist is the only one who can give you a real diagnosis, but recognizing the signs that your “everyday stress” has morphed into persistent anxiety or a genuine mood disorder could make a life-changing difference.
When Stress Sticks: The Difference That Matters

What’s the simplest way to understand the difference?
Stress is typically tied to an external, specific trigger. That work deadline or the argument? That’s stress. When the outside pressure lifts, the intense emotional response usually dissipates as well.
Conversely, a mental health condition (like an anxiety disorder, depression, or even burnout) is internal and persistent. It’s a state that sticks around, even when there’s no clear, obvious reason for it. Your body effectively gets stuck in high-alert mode. The initial reaction to a problem has, in fact, become the problem itself. This is when the real warning flares start to rise.
The Physical Symptoms of Stress We Love to Ignore
Our bodies are smarter than we give them credit for. They constantly try to signal when our system is overloaded. Unfortunately, most of us get incredibly good at tuning out the physical symptoms of stress.
We blame constant headaches on staring at the screen too long, or awful sleep on that one extra cup of coffee. When these symptoms start to pile up, though, it’s a clear sign you need to slow down. Are you noticing any of these?
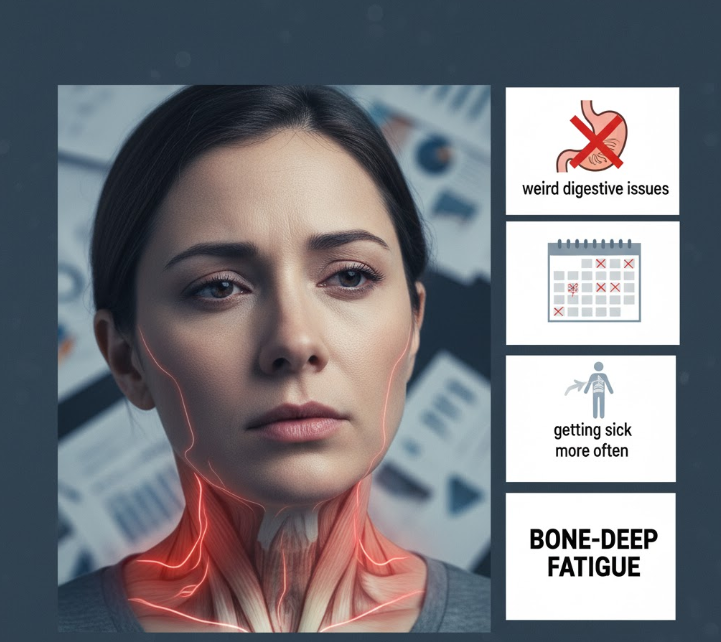
- Constant Muscle Tension: That stiffness in your neck, shoulders, and jaw seems to be a permanent feature now.
- Weird Digestive Issues: Your stomach just feels constantly “off,” upset, or persistently bothered by small things.
- Bone-Deep Fatigue: This is the critical one. You could get eight hours of sleep but still wake up feeling like you never even went to bed.
- That Persistent “Brain Fog”: Simple decisions, like what to make for dinner, feel impossible, and you can’t seem to hold a consistent focus.
- Getting Sick More Often: A system running on high stress fumes simply doesn’t have enough resources left to keep your immune system strong.
The Real Warning: When Stress Affects Your Daily Life

Here’s the single most important point you need to consider. The true indicator that something deeper is happening is when these feelings start to seriously interfere with the way you live your life.
This is the phase where you stop feeling like your normal self.
At first, it’s pretty subtle. Perhaps you start cancelling plans with friends—not because you’re busy with work, but because you simply can’t face it. Maybe you drop hobbies you used to genuinely love, or you stop going to the gym. Slowly, you find yourself isolating more and more.
When your day-to-day routine—your work, your relationships, even just basic tasks—begins to slip, that’s the symptom. It’s not laziness, and it’s certainly not a character flaw. It’s your system telling you it’s overloaded and needs support to function properly again.
Therapist vs. Psychiatrist: Who Should You See?

Admitting you need help and thinking, “Okay, now what?” can feel like a massive, vague step. One of the most common questions is: who do you even call first, a therapist or a psychiatrist?
It took me a while to understand the distinction when I first looked into it, but it’s actually pretty straightforward:
| Professional Type | Primary Role (The ‘What’) | Focus (The ‘How’) |
| Therapist (Psychologist, Counselor) | Provides talk therapy and counseling. | Helps you unpack why you feel this way. They offer tools, strategies, and coping skills. Think of it as managing the mental “software.” |
| Psychiatrist (M.D.) | Is a medical doctor who can diagnose and prescribe medication. | Manages the biological and chemical side of things. They handle the mental “hardware” and often focus on medication response. |
In reality, many people find the best results by seeing both—it’s not an either/or situation. The key, ultimately, is just to start the conversation with one of them.
Recognizing that you’re struggling isn’t a weakness; it’s honestly the bravest first step you can take toward feeling like your true self again. If any of this sounds familiar, I highly suggest just checking it out. You know your body and mind best, after all.
Reference Links
This article was written by reframing information without academic citations (e.g., [1], “According to~”), as strictly required by the blog guidelines. The following sources contain the key concepts and distinctions used in the content:
- Difference Between Stress, Anxiety, and Depression Symptoms:
- Physical Symptoms of Chronic Stress:
- Roles of Mental Health Professionals (Therapist vs. Psychiatrist):